What are the most common problems after cataract surgery?
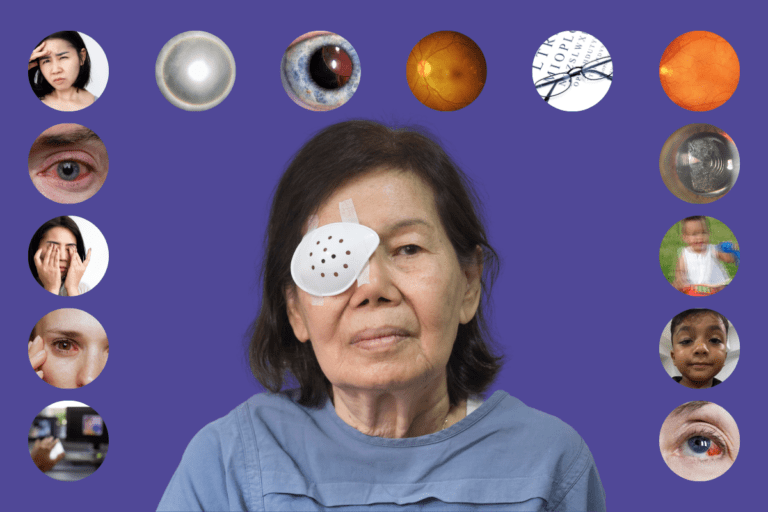
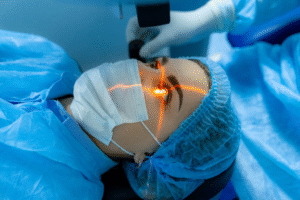
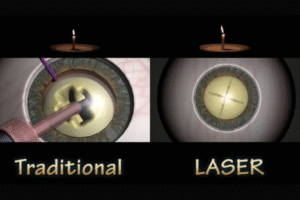
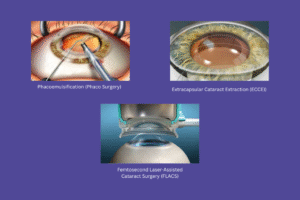
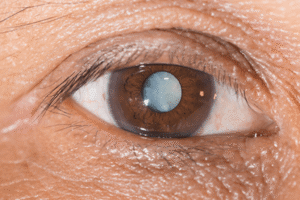
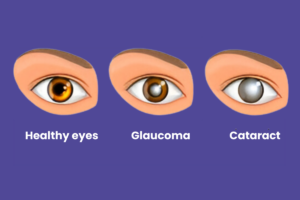
Cataract surgery is one of the most commonly performed procedures in the world, with a high success rate. It involves the removal of the clouded natural lens in the eye and replacing it with an artificial intraocular lens (IOL). Most patients experience significant improvement in their vision following the procedure, but as with any surgery, there can be potential risks and complications in the post-surgery period.
Understanding what to expect and how to manage any issues that arise can help ensure a smooth recovery. In this blog, we’ll discuss the most common problems patients might experience after cataract surgery, along with tips on how to manage them.
- Blurred vision
- Dry eyes
- Eye infection
- Inflammation
- Increased light sensitivity
- Glare & Halos
- Dislocated or Shifted Intraocular Lens (IOL)
- Retinal detachment
- Overcorrection or Undercorrection of vision
- Cystoid Macular Edema (CME)
- Posterior Capsular Opacification (PCO)
- Fluctuating vision
- Ptosis (Drooping eyelid)
- Ocular hypertension
Table of Contents
Toggle1. Blurred vision

- What it is: After cataract surgery, it is common for patients to experience blurred or cloudy vision in the initial days or even weeks.
- Cause: This happens because the eye is healing, and the brain is adjusting to the new lens.
- How to manage: Blurred vision usually resolves itself as the eye continues to heal. It’s important to follow your doctor’s instructions for post-surgery care, including the use of prescribed eye drops.
- When to seek help: If blurred vision persists for more than a few weeks or worsens, it could indicate another issue, such as an infection or a dislocated lens. Contact your surgeon for a follow-up.
2. Dry eyes

- What it is: Many patients experience a feeling of dryness, itchiness, or a gritty sensation in the eyes after cataract surgery.
- Cause: Cataract surgery temporarily disrupts the eye’s ability to produce tears, which can lead to dry eye symptoms.
- How to manage: Use lubricating eye drops as prescribed by your doctor to relieve the discomfort. Avoid smoke, dust, and other irritants that can exacerbate dryness.
- When to seek help: If symptoms of dry eyes become severe or persistent, or if they don’t improve with lubricating drops, it’s essential to consult your eye doctor.
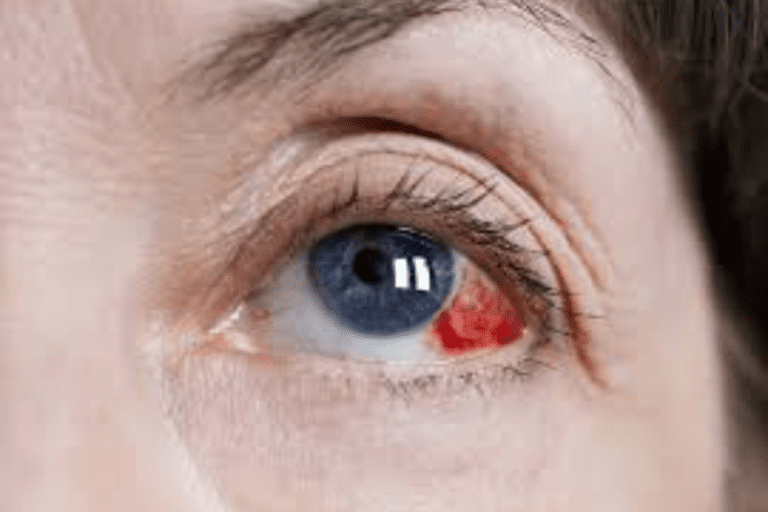
3. Eye infection

- What it is: Infections are one of the more serious complications that can occur after cataract surgery, though they are rare.
- Cause: Infection can develop if bacteria enter the eye during surgery or if proper hygiene isn’t maintained during the recovery period.
- How to manage: Follow all prescribed guidelines for hygiene, including avoiding rubbing your eyes, and take all medications as directed.
- When to seek help: If you notice increased redness, swelling, pain, or discharge from the eye, seek medical help immediately, as these may be signs of an infection.
4. Inflammation
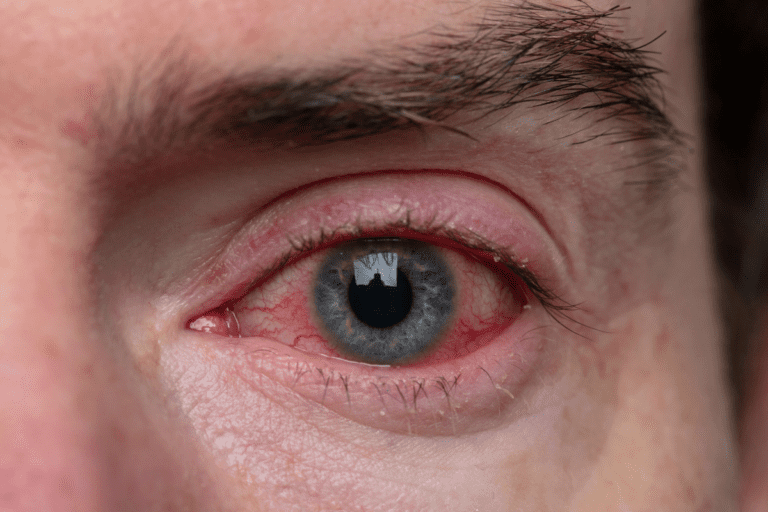
- What it is: Some inflammation in the eye is normal after cataract surgery, but it can cause discomfort and redness.
- Cause: This is a natural part of the healing process as the body works to repair the surgical site.
- How to manage: Your doctor will likely prescribe anti-inflammatory eye drops to manage this issue. These will help reduce swelling and discomfort.
- When to seek help: If inflammation becomes severe or persists despite using the prescribed medication, it could signal an issue that requires further evaluation.
5. Increased light sensitivity

- What it is: After cataract surgery, patients often experience heightened sensitivity to light, which may cause discomfort in bright environments.
- Cause: The eye is adjusting to the new lens, and the removal of the cataract can make the eye more sensitive to light.
- How to manage: Wearing sunglasses or avoiding bright light during the recovery period can help. Many patients find that this issue improves as their eye heals.
- When to seek help: If light sensitivity continues for an extended period or worsens, consult your doctor to ensure proper healing.
6. Glare & Halos

- What it is: Some patients notice glare or halos around lights, especially at night, after cataract surgery.
- Cause: The intraocular lens (IOL) may alter how light enters the eye, leading to this visual disturbance.
- How to manage: This issue often improves over time as the eye adapts to the IOL. In the meantime, wearing glasses with an anti-reflective coating can help reduce glare.
- When to seek help: If glare and halos are particularly bothersome or worsen over time, speak with your ophthalmologist. In some cases, further intervention may be needed.
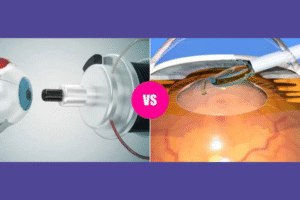
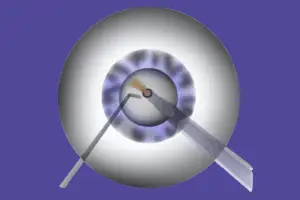
7. Dislocated or Shifted Intraocular Lens (IOL)
- What it is: Rarely, the IOL can become dislocated or shift from its original position, leading to blurred vision.
- Cause: This can occur due to improper placement during surgery or other factors such as trauma to the eye.
- How to manage: If an IOL shift occurs, it may be possible to reposition the lens surgically.
- When to seek help: If your vision becomes blurry or distorted after the initial improvement, it’s important to contact your surgeon for an evaluation.
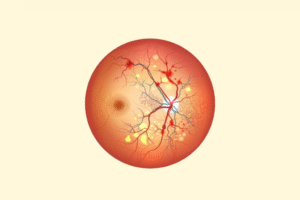
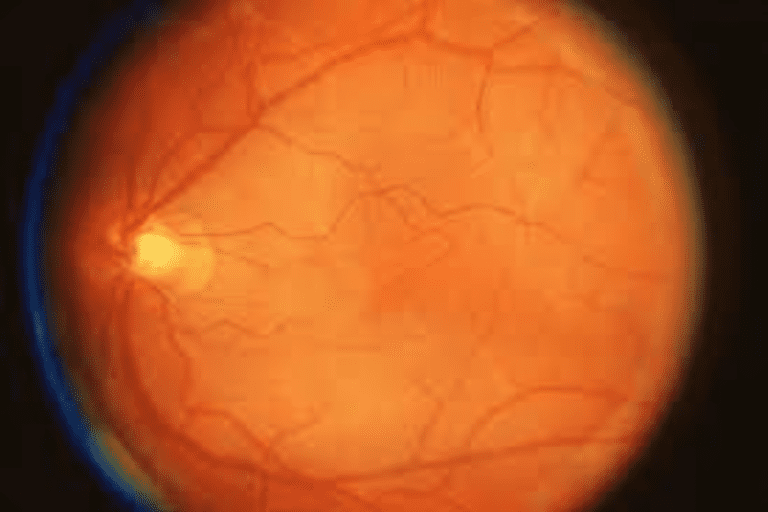
8. Retinal detachment

- What it is: Retinal detachment is a rare but serious complication that can cause permanent vision loss if not treated promptly.
- Cause: The retina may begin to detach from the back of the eye after cataract surgery, typically due to changes in the eye’s structure.
- How to manage: Retinal detachment usually requires immediate surgical repair.
- When to seek help: If you experience flashes of light, a sudden increase in floaters, or a shadow in your field of vision, seek emergency medical attention.
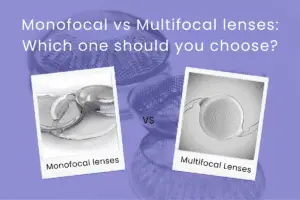
9. Overcorrection or Undercorrection of vision

- What it is: Some patients may still need glasses or contact lenses for certain activities like reading or driving.
- Cause: In some cases, the IOL may not provide the precise level of correction needed for optimal vision.
- How to manage: This can often be corrected with prescription glasses or contact lenses. In some cases, a secondary procedure may be necessary to fine-tune the results.
- When to seek help: If you notice persistent vision issues despite corrective lenses, your doctor may recommend an additional procedure to address the issue.
10. Cystoid Macular Edema (CME)
- What it is: CME is a condition where the central part of the retina (the macula) swells, impairing central vision.
- Cause: It may develop after cataract surgery due to inflammation within the eye.
- How to manage: CME can usually be treated with anti-inflammatory medications, and patients will be monitored closely to track progress.
- When to seek help: If you notice a decrease in your central vision or blurry spots in your line of sight, contact your eye care provider.
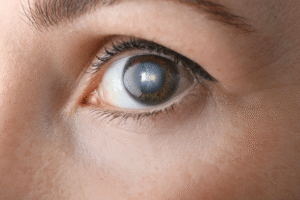
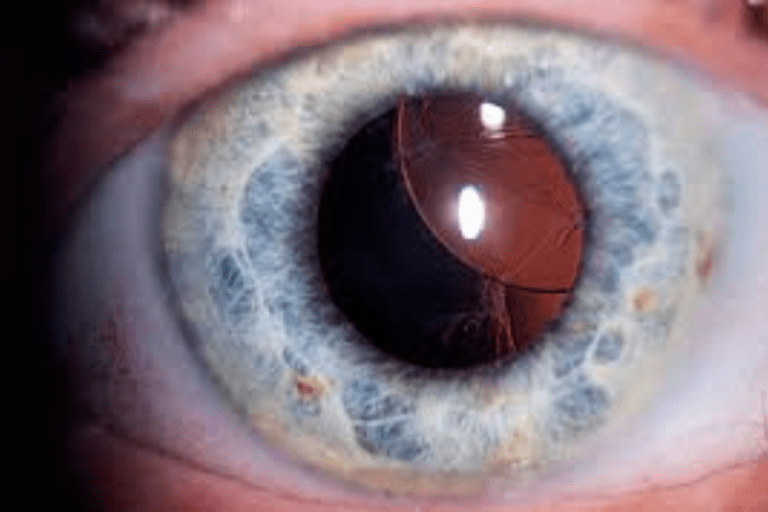
11. Posterior Capsular Opacification (PCO)
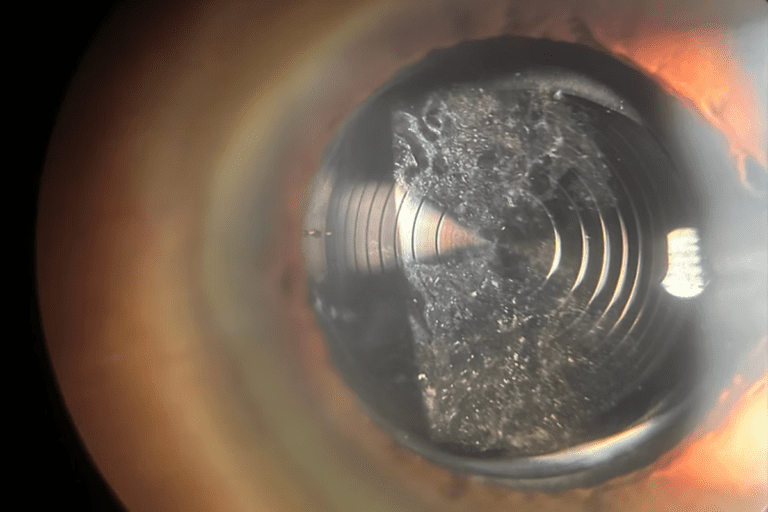
- What it is: PCO is a condition where the back of the lens capsule becomes cloudy, which can cause blurred vision after cataract surgery.
- Cause: This happens when cells from the original cataract tissue grow on the lens capsule.
- How to manage: PCO can be treated with a simple laser procedure called YAG laser capsulotomy, which is quick and painless.
- When to seek help: If your vision begins to blur again after initial improvement, you may have developed PCO and should consult your doctor for treatment.
12. Fluctuating vision

- What it is: Some patients experience fluctuating vision, where the quality of their vision changes throughout the day.
- Cause: This can happen due to eye dryness or as part of the healing process.
- How to manage: Staying hydrated, using prescribed eye drops, and resting your eyes periodically can help.
- When to seek help: If fluctuations persist or worsen beyond a few weeks, further evaluation may be needed.
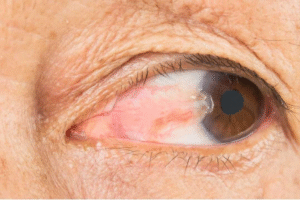
13. Ptosis (Drooping eyelid)

- What it is: Ptosis refers to the drooping of the upper eyelid, which can occur after cataract surgery.
- Cause: This can happen due to swelling or changes in the eye muscles following surgery.
- How to manage: Most cases resolve on their own, but if ptosis is significant, treatments or surgery may be needed.
- When to seek help: If ptosis is severe or doesn’t improve over time, consult your surgeon for further evaluation.
14. Ocular hypertension
- What it is: Ocular hypertension refers to increased pressure inside the eye, which can lead to glaucoma if not managed properly.
- Cause: Some patients may experience elevated intraocular pressure (IOP) after cataract surgery.
- How to manage: Regular monitoring of eye pressure and prescribed medications to control pressure are essential.
- When to seek help: If you experience symptoms like eye pain, headache, or blurry vision, consult your doctor immediately.
Conclusion
While cataract surgery is highly effective and offers life-changing improvements in vision, it’s essential for patients to be aware of the potential complications that can arise in the post-operative period. Most issues are temporary and manageable with proper care and follow-up. If you experience any unusual symptoms or persistent problems, always reach out to your ophthalmologist at Krisha Eye Hospital for guidance. Early detection and intervention can help ensure the best possible outcome from your surgery.
At Krisha Eye Hospital, we are dedicated to providing the highest quality care and support throughout your recovery journey. If you have any concerns or questions, don’t hesitate to contact us.
Author bio
Dr. Dhwani Maheshwari, an esteemed ophthalmologist with over 10 years of experience, leads Krisha Eye hospital in Ahmedabad with a commitment to advanced, patient-centered eye care. Specializing in cataract and refractive surgery, Dr. Maheshwari has performed more than a thousand successful surgeries. Her expertise lies in phacoemulsification, a technique recognized for its precision in cataract treatment.
Dr. Maheshwari’s educational journey includes an MBBS from Smt. NHL MMC, a DOMS from M & J Institute of Ophthalmology, and a DNB in Ophthalmology from Mahatme Eye Bank Eye Hospital, Nagpur. She also completed a fellowship in phacoemulsification at Porecha Blindness Trust Hospital, further enhancing her surgical skills. In addition to her work at Krisha Eye Hospital, Dr. Maheshwari serves as a consultant ophthalmologist at Northstar Diagnostic Centre.
Under her leadership, Krisha Eye Hospital aims to bring all superspecialties under one roof, offering comprehensive eye care solutions for all vision needs.
FAQs
Yes, some blurred vision is normal in the first few days or weeks after cataract surgery as the eye heals. It may also occur as your brain adjusts to the new intraocular lens (IOL). However, if blurred vision persists beyond the expected recovery period, it’s important to contact your doctor.
Dry eyes are a common issue after cataract surgery. This can last for a few weeks to months as the eye heals and adjusts. Your surgeon will likely recommend lubricating eye drops to relieve the discomfort. If dry eye symptoms are severe or don’t improve, it’s important to follow up with your ophthalmologist.
While mild discomfort is normal, severe pain may indicate a complication, such as infection or inflammation. If you experience intense pain, redness, or swelling in the eye, contact your doctor immediately to ensure prompt treatment.
To prevent infection, follow hygiene instructions carefully. Avoid touching or rubbing your eyes, especially with unwashed hands. Always take the prescribed antibiotic eye drops as directed and avoid exposure to dust, smoke, or other potential irritants.
While it’s rare, the IOL can sometimes shift from its original position. If this occurs, it may lead to blurred vision. If you notice any changes in your vision or discomfort, contact your surgeon. They can assess the position of the IOL and recommend appropriate treatment.
Halos and glare are common visual disturbances in the early recovery phase after cataract surgery. These occur because the new lens is still adjusting to your eye, especially in low-light conditions. This usually improves over time, but if it persists or worsens, discuss it with your ophthalmologist.
Most patients can resume normal activities such as reading or light work within a few days to a week. However, strenuous activities like heavy lifting or swimming should be avoided for at least 4-6 weeks to allow your eye to fully heal. Always follow your surgeon’s recommendations regarding activity restrictions.
Fluctuating vision is common in the early stages of recovery. It can be due to factors such as healing of the eye, dry eyes, or the brain adjusting to the new IOL. If vision fluctuations persist or worsen, consult your doctor for further evaluation.
Contact your doctor if you experience any of the following symptoms:
- Severe pain or discomfort.
- Increased redness, swelling, or discharge from the eye.
- Blurry or fluctuating vision that doesn’t improve over time.
- Flashes of light, a sudden increase in floaters, or a shadow in your vision (signs of retinal detachment).
Persistent glare or halos that interfere with daily activities.
Full recovery can take several weeks to months, depending on the individual. Most patients notice significant improvements in vision within the first few days to weeks, but minor adjustments, such as fluctuating vision or dryness, may continue for a longer period. Regular follow-up appointments with your surgeon are crucial for monitoring progress. You can learn more about the recovery timeline in our detailed guide.