Cataract surgery in patients with glaucoma
Cataracts and glaucoma are two common eye conditions that can significantly impact vision, particularly in older adults. When both conditions are present in the same patient, managing them becomes more complex. With careful evaluation and an individualized treatment plan, cataract surgery can be safely performed in patients with glaucoma to achieve better visual outcomes and maintain long-term eye health
In this blog, we’ll explore how cataract surgery is performed in glaucoma patients, the risks involved, and the combined treatment approaches available.
Table of Contents
ToggleUnderstanding cataracts and Glaucoma
Cataracts
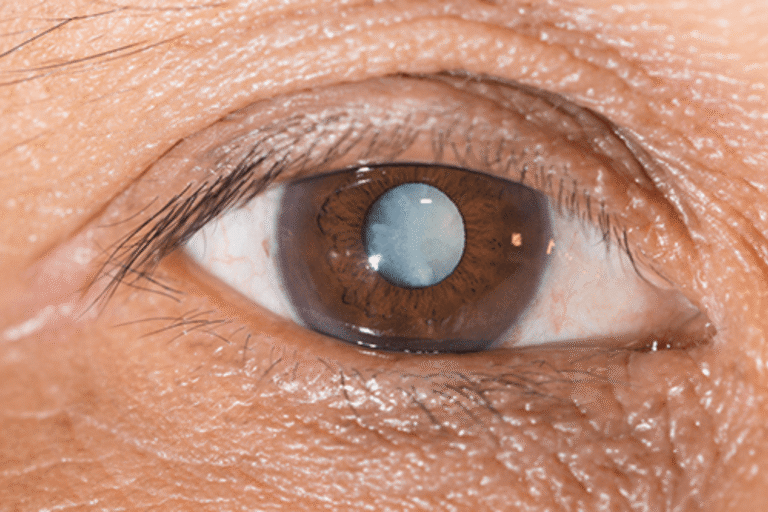
A cataract is the clouding of the eye’s natural lens, leading to blurred vision, glare, difficulty seeing at night, and dullness in color perception. Cataracts typically progress with age and are treated effectively through surgery that replaces the cloudy lens with a clear artificial intraocular lens (IOL).
Glaucoma
Glaucoma is a group of eye diseases that damage the optic nerve, usually due to high intraocular pressure (IOP). It can lead to irreversible vision loss if left untreated. Glaucoma can be open-angle, angle-closure, or secondary to other eye conditions.
Can cataract surgery be done in glaucoma patients?
Yes. In fact, cataract surgery can sometimes help lower eye pressure in patients with certain types of glaucoma. However, it requires careful planning and a tailored approach, especially in patients with advanced glaucoma or those on multiple medications.
Special considerations before surgery
- Detailed eye examination
- Visual field testing and OCT scans of the optic nerve.
- IOP measurements and medication assessment.
- Gonioscopy to evaluate the drainage angle.
- Visual field testing and OCT scans of the optic nerve.
- Timing of Surgery
- In some cases, cataract surgery is done before glaucoma becomes severe to improve IOP control.
- In other cases, both cataract and glaucoma surgeries are combined in a single procedure.
- In some cases, cataract surgery is done before glaucoma becomes severe to improve IOP control.
- Type of glaucoma
- Patients with angle-closure glaucoma often benefit significantly from cataract surgery alone.
- In open-angle glaucoma, the surgery might lower IOP modestly but may not eliminate the need for medications.
- Patients with angle-closure glaucoma often benefit significantly from cataract surgery alone.
Surgical options
1. Standalone cataract surgery
- In patients with well-controlled glaucoma on medications.
- May slightly reduce IOP due to improved aqueous outflow.
2. Combined cataract and Glaucoma surgery
- Suitable for patients with uncontrolled glaucoma or who are on multiple medications.
- Types of combined surgeries:
- Phacoemulsification + Trabeculectomy
- Phacoemulsification + Glaucoma Drainage Device (e.g., Ahmed valve)
- Phacoemulsification + Trabeculectomy
Phacoemulsification + MIGS (Minimally Invasive Glaucoma Surgery) like iStent, Hydrus
3. Minimally Invasive Glaucoma Surgery (MIGS)
- Less invasive procedures performed alongside cataract surgery.
- Shorter recovery, fewer complications.
- Ideal for mild to moderate glaucoma.
Intraocular Lens (IOL) selection
- Monofocal IOLs are usually preferred to ensure good quality of vision.
- Multifocal or toric lenses may be avoided in patients with advanced glaucoma due to reduced contrast sensitivity or optic nerve damage.
Post-Surgical care
- Regular Monitoring of Eye Pressure.
- Adjusting or Continuing Glaucoma Medications.
- Avoiding Eye Strain or Pressure Post-Surgery.
- Follow-Up Visual Field and OCT Testing.
Potential risks and Complications
- Fluctuations in IOP after surgery.
- Risk of glaucoma worsening in advanced cases.
- Risk of bleb failure in previous trabeculectomy patients.
- In rare cases, optic nerve damage due to sudden IOP changes.
However, with proper planning and skilled surgical care, these risks are significantly minimized.
Benefits of cataract surgery in glaucoma patients
- Improved visual clarity.
- Reduced dependence on glaucoma drops. (in some cases)
- Better quality of life.
- Option to combine surgeries and reduce treatment burden.
Conclusion
Cataract surgery in patients with glaucoma is not only possible—it can often improve both vision and eye pressure control. However, the approach must be carefully tailored to the patient’s condition. At Krisha Eye Hospital in Ahmedabad, our experienced ophthalmologists perform comprehensive evaluations and use the latest techniques in cataract and glaucoma surgery to ensure the best possible outcomes.
If you or a loved one has both cataracts and glaucoma, don’t delay treatment. Book a consultation with our experts today to explore the safest and most effective surgical plan.
Author bio
Dr. Dhwani Maheshwari, an esteemed ophthalmologist with over 10 years of experience, leads Krisha Eye hospital in Ahmedabad with a commitment to advanced, patient-centered eye care. Specializing in cataract and refractive surgery, Dr. Maheshwari has performed more than a thousand successful surgeries. Her expertise lies in phacoemulsification, a technique recognized for its precision in cataract treatment.
Dr. Maheshwari’s educational journey includes an MBBS from Smt. NHL MMC, a DOMS from M & J Institute of Ophthalmology, and a DNB in Ophthalmology from Mahatme Eye Bank Eye Hospital, Nagpur. She also completed a fellowship in phacoemulsification at Porecha Blindness Trust Hospital, further enhancing her surgical skills. In addition to her work at Krisha Eye Hospital, Dr. Maheshwari serves as a consultant ophthalmologist at Northstar Diagnostic Centre.
Under her leadership, Krisha Eye Hospital aims to bring all superspecialties under one roof, offering comprehensive eye care solutions for all vision needs.
FAQs
Yes, most patients need to continue their glaucoma medications after surgery, at least temporarily. Your doctor will guide you based on your eye pressure readings post-surgery.
It depends. Some patients experience improved IOP control after cataract surgery, while others may still require glaucoma surgery later on.
Most patients can resume light activities within a few days. However, those with glaucoma may need extra monitoring and follow-up before returning to strenuous activities.
While cataract removal can improve vision clarity, it does not restore the visual field lost due to glaucoma. However, it can make visual field testing more accurate postoperatively.
There may be slightly increased risks due to existing optic nerve damage or prior glaucoma surgeries, but with proper planning, outcomes are usually favorable.
In rare cases, eye pressure may rise significantly after surgery, potentially affecting glaucoma. Regular monitoring helps detect and manage such issues early.
